By Dr Patrick Sokiri
While moderating sessions at the 10th East African Health and Scientific Conference in Juba, a distressing video began to circulate. It showed a gang rape reportedly committed in Sherikat, Gumbo. The timing was jarring. As we hosted dignitaries, researchers, and policymakers to discuss health systems and scientific advancement, an act of unimaginable cruelty was unfolding just kilometers away.
Within days, another similar revenge video emerged. Same area. Another victim. Same chilling silence from the public and authorities.
It was in that moment that I found myself overwhelmed by a sense of lugubrious dismay. I was not just a doctor or public health practitioner standing before microphones and delegates. I was a South Sudanese witnessing the disintegration of community, identity, and accountability in real time.
Where Was Mental Health on the Agenda?
The Conference was well-organized. The discussions were rich. Yet amidst the plenary sessions on non-communicable diseases, universal health coverage, maternal and child health, and innovations in diagnostics, I did not hear a single substantive presentation on mental health.
Nothing on youth trauma.
Nothing on drug addiction.
Nothing on gang violence.
Not even a side event.
This is not a minor omission. It is a national oversight. Mental health is not a luxury. It is not a secondary concern. In post-conflict societies, it is the foundation for rebuilding human capital and peace.
South Sudan has the youngest population in East Africa and arguably the highest burden of trauma. Decades of war, displacement, sexual violence, poverty, and educational collapse have created a fertile ground for addiction, aggression, and hopelessness.
The current wave of gang activity and drug use is not random criminality. It is an untreated national mental health crisis.
Torit as a Case Study in Collapse
Earlier this month, I visited Torit to train HIV and AIDS change agents. It was personal. Torit is where my father was born. I lived there in the 1980s. We still have land in Malakia. I once stayed in Hai Turuju.
What I saw now was haunting.
Torit is not a war zone. But it is dying quietly.
Children abusing tramadol.
Youth gangs openly recruiting boys as young as twelve.
Alcohol sold at every corner.
No mental health outreach. No psychosocial services. No safe spaces for rehabilitation.
The most active public spaces were pharmacies selling sedatives without prescriptions.
How does a society survive this?
The Failure Is Systemic
South Sudan’s Community Mental Health Strategy (2024–2028) is a commendable policy document. But without funding, training programs, cross-sector coordination, and community involvement, it remains a file in a cabinet.
We have no national mental health referral center.
No structured addiction treatment network.
Very few trained psychiatrists, psychologists, or psychiatric nurses.
Little to no postgraduate mental health training for public health officers or clinical officers.
Yet we are witnessing:
Rising youth suicide
Gender-based violence
Drug-induced psychosis
School dropout
Family disintegration
Urban gang expansion
Mental health is no longer a clinical issue. It is a governance issue. A peacebuilding issue. A national development issue.
What Must Be Done Immediately
1. Declare Mental Health a National Development Priority
The Ministry of Health, Ministry of Youth, Ministry of Interior, and Ministry of Higher Education must jointly recognize the crisis. Coordination is essential.
2. Establish a National Mental Health and Addiction Center in Juba
With branches in Wau, Torit, and Malakal. These centers must provide detox, psychosocial counseling, and community-based rehabilitation.
3. Fund Postgraduate Mental Health Education
Support postgraduate diplomas and master’s programs for mental health professionals in South Sudan and across East Africa.
4. Integrate Mental Health into Primary Health Care
Train all primary health workers in mental health screening and first-line support. Equip facilities with basic psychotropic medicines and referral tools.
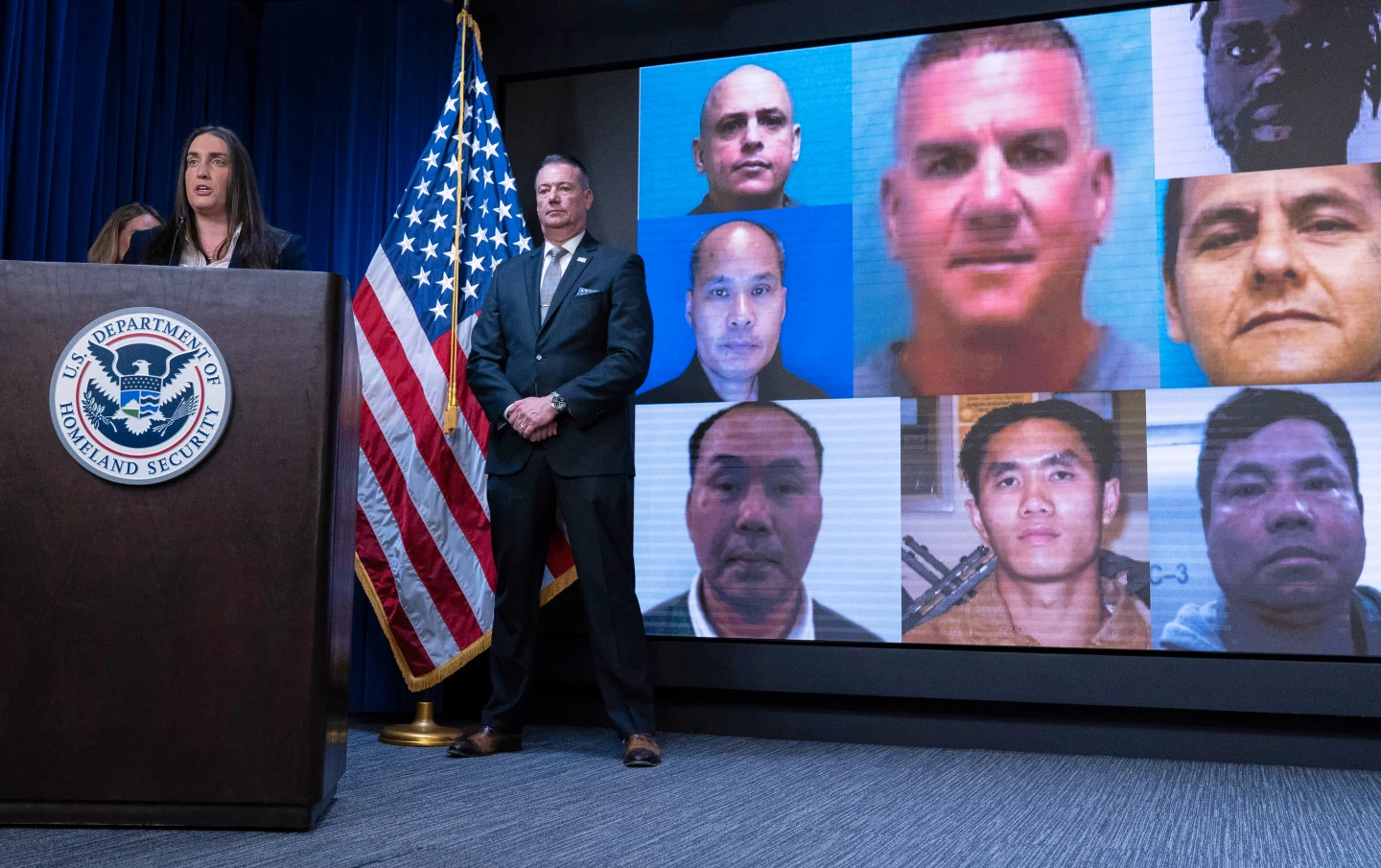
5. Tackle Gang Violence as a Mental Health Outcome
Establish early-warning systems in schools and communities. Offer diversion programs for at-risk youth. Include trauma recovery and family counseling.
6. Reform Pharmacy Regulation and Drug Supply Chains
The South Sudan Pharmacy Board must act. Tramadol, diazepam, and cough syrups with psychoactive ingredients are flooding towns unchecked.
7. Engage Religious and Cultural Leaders in Healing Work
Mental health must be demystified through culturally sensitive messaging. Let mosques, churches, and traditional institutions lead community recovery efforts.
Call to the East African Community
South Sudan is the youngest member of the East African Community. The region cannot afford to watch its newest member bleed in silence.
I urge the EAC Secretariat, the East African Health Research Commission, and regional universities to:
Support South Sudan in building a national mental health workforce
Facilitate regional research collaboration and data collection
Include mental health and youth violence in all upcoming health conferences
Provide scholarships for South Sudanese clinicians and public health workers in psychiatry, psychology, and addiction medicine
Fund community pilot programs for psychosocial support in post-conflict settings
South Sudan’s challenges are regional challenges. If left unaddressed, this crisis will export insecurity, migration, and trauma to its neighbors.
If We Do Not Intervene, We Are Complicit
The girl in Sherikat is not just a victim of a gang. She is a victim of state failure. Of societal breakdown. Of our collective silence.
The boy in Torit is not just a drug addict. He is a casualty of institutional neglect. A reflection of unhealed trauma.
We cannot call ourselves health professionals, policymakers, or regional actors and ignore what is happening.
The future of South Sudan lies not only in infrastructure or elections. It lies in the minds of its youth.
If we do not treat those minds, we will lose the nation.
Dr Patrick Sokiri is a physician and public health activist. He is a humanitarian worker with over 15 years working in South Sudan and sub Saharan Africa at an international setting.